Sudden cardiac death (SCD) is a devastating tragedy, particularly when it can be prevented. The American Heart Association (AHA) recommends a 14-point evaluation for sports physicals, which includes questions on symptoms and family history, as well as blood pressure measurements, height, and weight. In addition, the heart is listened to in multiple positions, and there is an examination for physical stigmata of Marfan syndrome. If there are any concerns about the medical history or exam, an ECG or transthoracic echocardiogram (TTE) is then performed [1]. Please review the sports physical form.
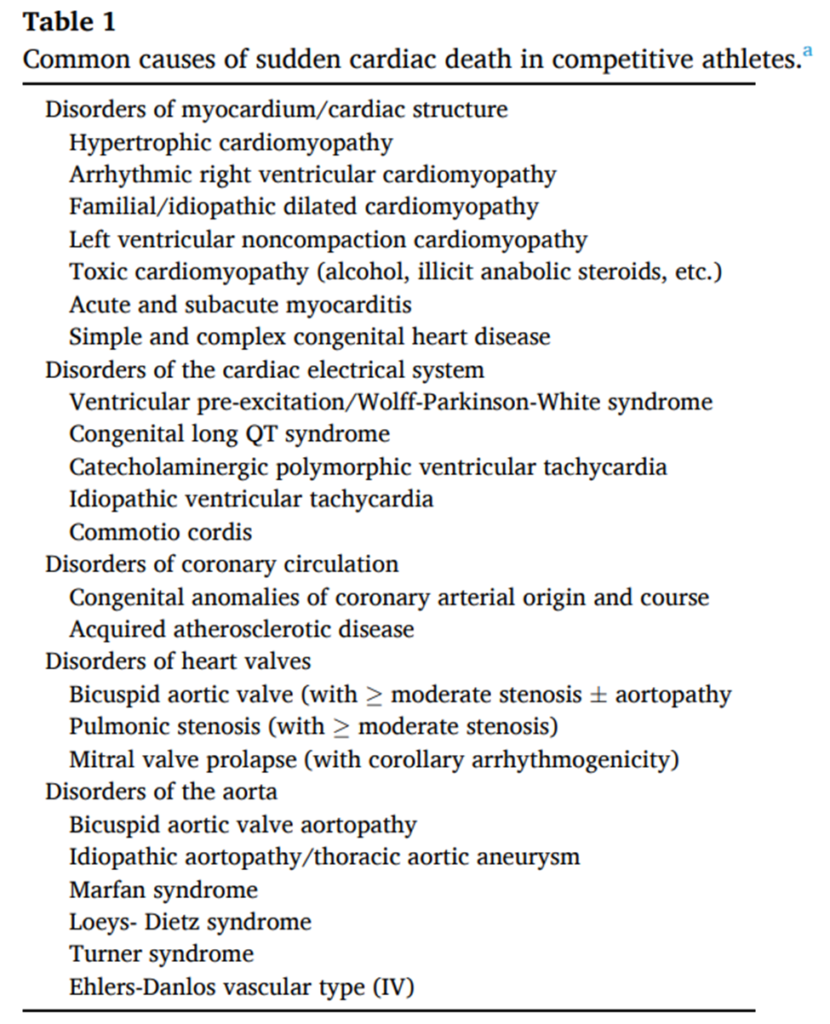
What are the Common Cardiac Causes of Sudden Cardiac Death in Athletes?
There are several common cardiac causes of sudden cardiac death in athletes, including long QT syndrome, Wolf-Parkinson-White syndrome (WPW), hypertrophic cardiomyopathy (HCM), dilated cardiomyopathy, cardiac contusion/commotio, arrhythmogenic right ventricular cardiomyopathy, myocarditis, aortic valve stenosis/regurgitation, outflow tract obstructions, subaortic membrane, coronary artery disease, anomalous coronary arteries, and hypertension [2]. See table 1 for more common causes.
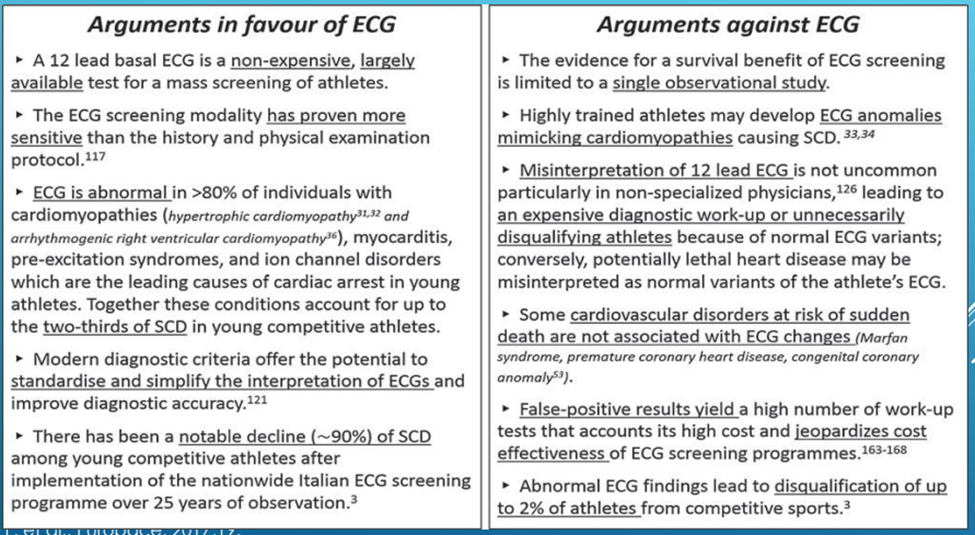
The Argument to Include Electrocardiograms (ECGs)
Multiple studies have shown that ECGs can vastly aid in screening young athletes for SCD. The AHA 14-point evaluation, which is inexpensive, has poor sensitivity as most athletes are asymptomatic. Thus, the H&P only identifies a minority of those athletes at risk for SCD. From William E et al., the sensitivity (18.8%), specificity (68.0%), and positive predictive value (0.3%) of the AHA 14-point evaluation was substantially lower than the sensitivity (87.5%), specificity (97.5%), and positive predictive value (13.6%) of ECG [2].
In Italy, ECGs are mandated by law and have been part of the European screening since research in Italy showed almost a 90% drop in SCD in their athletes [3]. The European Society of Cardiology recommends including the ECG with the screen as it improves sensitivity for detecting serious cardiac disease. A meta-analysis by Harmon et al. showed that compared to the H&P alone, adding ECGs to screening is six times more likely to detect a cardiovascular condition associated with SCD than without [4].

Research supporting EKG
A study at the University of Washington, sponsored by Nick of Time Foundation, showed that with the AHA 14-point evaluation, a positive H&P does not appear to identify a subgroup of athletes at higher risk of an underlying pathologic cardiac disorder. In contrast, this study suggests that 1 of every seven athletes flagged with an abnormal ECG will have a condition associated with SCD [2].
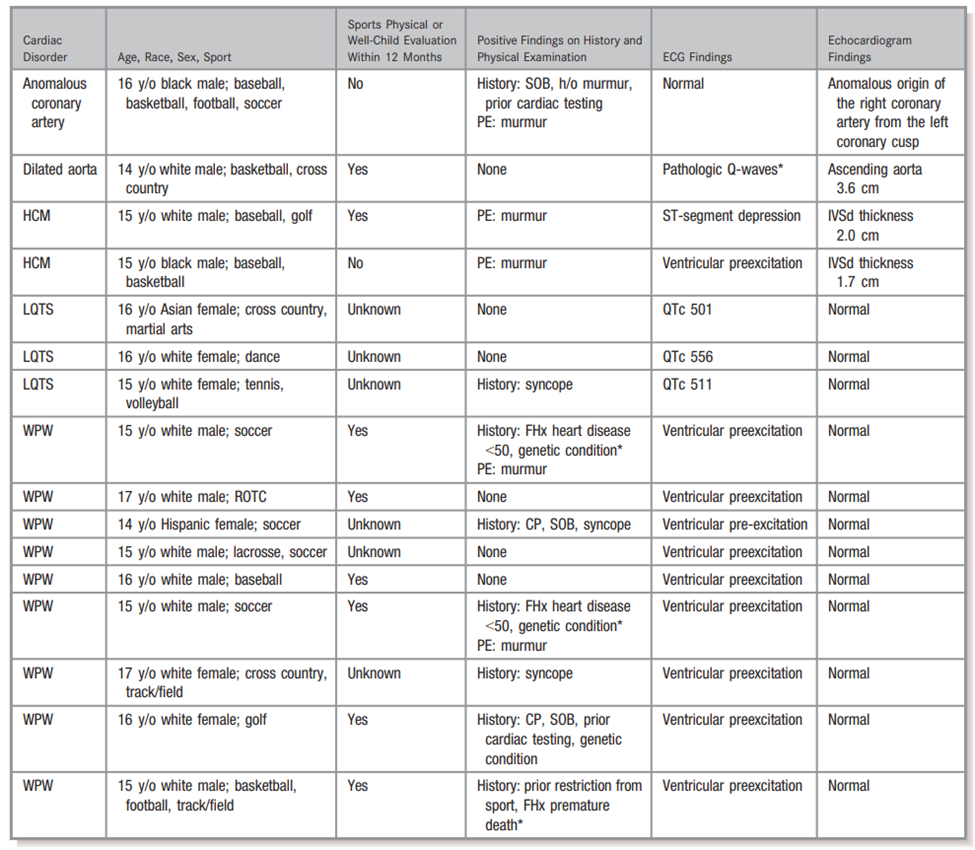
The study comprised 3620 student-athletes. Sixteen (0.4%) had significant cardiac conditions associated with SCD (Table 2). Nine athletes had Wolff-Parkinson-White, 3 had long QT syndrome, 2 had hypertrophic cardiomyopathy, 1 had a dilated aorta, and 1 had an anomalous origin of the right coronary artery. The AHA 14-point evaluation was flagged as abnormal in 7 of 16 (43.8%) cases. The ECG was flagged as abnormal in 15 of 16 (93.8%) cases. No athlete was identified with a cardiac condition associated with SCD solely from an abnormal physical examination.
If the AHA 14-point evaluation (positive questionnaires and abnormal physical exam) were the only screening tool to trigger further cardiac testing with an ECG and echocardiogram, 9 of 16 (56.2%) cases would remain undetected, including 3 Wolff-Parkinson-White, 3 long QT syndrome, 2 hypertrophic cardiomyopathy, and 1 dilated aorta. If ECG were the only screening tool to trigger further cardiac testing, only 1 of 16 (6.2%) cases would remain undetected (anomalous coronary artery) [2].
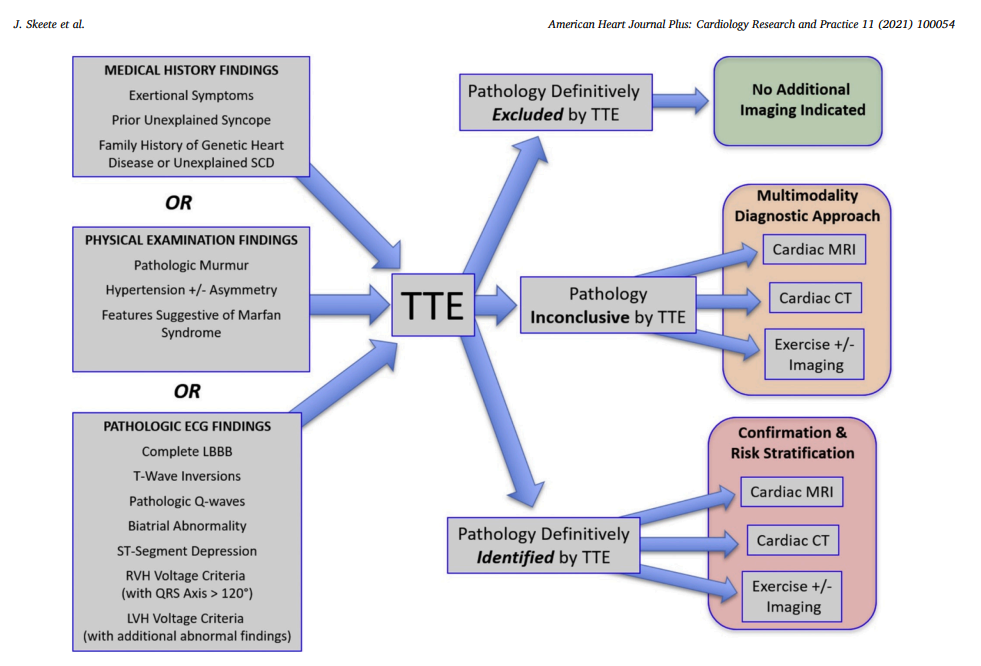
Why Include Transthoracic Echocardiogram (TTE)?
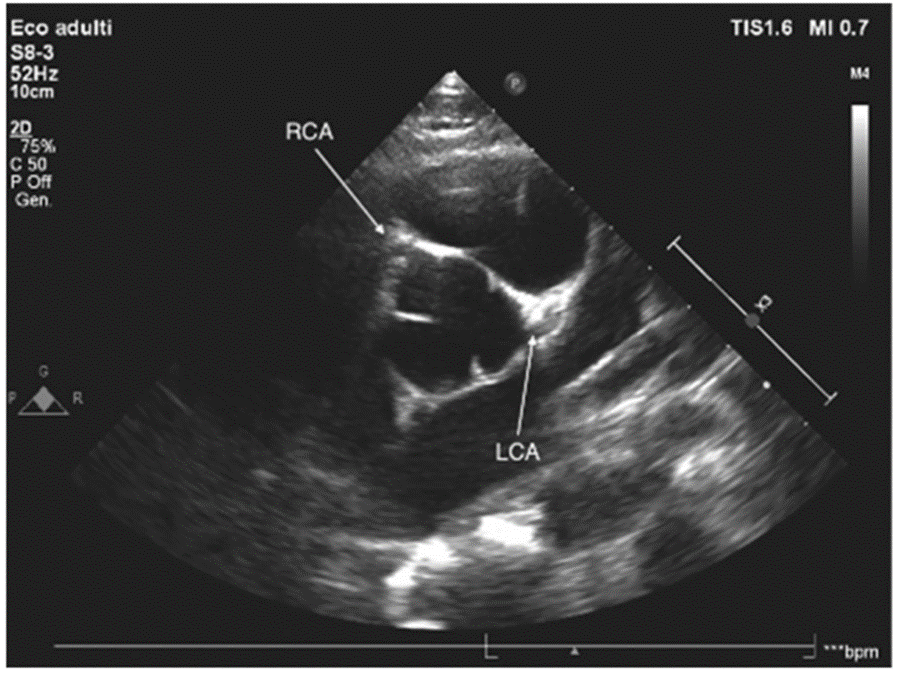
Transthoracic echocardiogram, also known as heart ultrasound, has emerged as a valuable diagnostic modality for assessing various cardiac conditions. Bronzetti et al. recommend it as a potential screening option for Sudden Cardiac Death (SCD) in settings where additional screening is available. With the assistance of a skilled interpreter, echocardiography offers accurate identification of bicuspid aortic valve, aortopathy, valvular disease, pathologic cardiomyopathies, and congenital heart disease.
Furthermore, echocardiographic images can guide further evaluation and management of competitive athletes with electrocardiograms suggestive of hypertrophic cardiomyopathy. Although identifying the origins of coronary arteries is not a standard component of most adult echocardiography protocols in the United States, the procedure is feasible. It can supplement existing echocardiographic assessments [5]. It is particularly significant in pediatric cardiology, where it is part of the protocol. Hence, transthoracic echocardiogram is a critical diagnostic tool for evaluating various cardiac conditions. Healthcare providers can rely on this non-invasive procedure to offer crucial insights into the cardiac structure and function and guide appropriate management strategies.
International support with adding both EKG and echocardiogram

While the AHA is debating recommending 12-lead ECG to the sports screen, major international sporting federations have mandated ECG and echocardiogram for their athletes (table 3). Different tests aid in the diagnosis of potential causes of sudden cardiac death. ECGs look at the electrical system, while echocardiograms evaluate the structures and can pick up abnormalities that ECGs miss (see Table 4).
| Causes of Sudden Death | Current screening – Questionnaires on symptoms, family history, and cardiac exam to determine the probability of heart disease and if further testing is needed. | ECG – look at electrical conduction | Echocardiogram with ECG leads – look at the structure and rhythm during the study |
| Long QT | The patients may be asymptomatic and not get picked up. A murmur may suggest obstruction to blood flow. | Abnormal | Abnormal on ECG leads |
| WPW | Abnormal | Can be abnormal on ECG leads | |
| Brugada | Abnormal | Normal | |
| Hypertrophic Cardiomyopathy | Abnormal | Abnormal | |
| Dilated cardiomyopathy | Possible | Abnormal | |
| Arrhythmogenic right ventricular cardiomyopathy | Abnormal (subtle sign) | Abnormal | |
| Cardiac contusion/commotio (sudden blow to chest) | Abnormal- arrhythmia | Abnormal | |
| Anomalous coronary arteries | Can be normal | Abnormal | |
| Outflow tract obstructions (valvulopathies) | It can be normal unless significant. | Abnormal | |
| Aortic dilation (aortopathy) | Can be normal | Abnormal |
Why the US has not Recommended Adding ECG and TTE Despite the Data? The Debate Continues.
Despite its clear superiority over traditional screening, several arguments exist against widespread ECG screening.
| Argument in Favor of Transthoracic Echocardiogram (TTE) | Arguments Against Transthoracic Echocardiogram (TTE) |
|---|---|
| The heart is seen in real-time | Cost-effectiveness |
| Structural abnormalities are seen. | Limited human resources |
| Higher sensitivity | The potential downstream consequences of a FP(+) (misinterpreted) TTE |
| Noninvasive | Unknown if the use of TTE screening would translate to actual lives saved (more research needed) |
| Can evaluate the coronaries as ECG and H&P can be normal in patients with abnormal coronaries origin. |
Table 6. Pros and Cons of an Echocardiogram
What Next?
In conclusion, using H&P with ECG increases sensitivity and specificity compared to H&P alone, as it can detect more abnormalities. An echocardiogram can evaluate structures and coronaries, which ECG cannot. Most competitive athletes need to undergo screening with ECG and TTE, as they are usually asymptomatic. If parents do not have access to ECG or TTE, they should ask their child about chest pain, shortness of breath, irregular heartbeat, fainting with exercise, family history of members dying from a heart condition under 50 years old, or history of Marfan’s or connective tissue disorder. If the child’s cardiac exam is abnormal, further evaluation is necessary. Talk to your doctor about sports screens and specific concerns.
To schedule an appointment, please get in touch with us at [email protected] or visit our website. We maintain transparency and affordability in our procedures and testing. Our clinic promotes a culture where children can play hard and enjoy activities to the fullest while ensuring their safety. We understand the importance of physical activity for children and its many benefits, from improving overall health to developing social skills and boosting self-confidence. However, we also recognize the potential risks of certain activities and sports. Therefore, we prioritize prevention and support heart health. We aim to create an environment where children can have fun, stay active, and thrive while playing safely.
This post is to provide information and opinion. It is not medical advice. Please discuss individual questions/concerns with your doctor.
References:
- Skeete J et al., Preventing sudden cardiac death in young athletes – A perspective from the United States, American Heart Journal Plus: Cardiology Research and Practice, Volume 11, 2021, 100054, ISSN 2666-6022, https://doi.org/10.1016/j.ahjo.2021.100054.
- Williams E et al., Performance of the American Heart Association (AHA) 14-Point Evaluation Versus Electrocardiography for the Cardiovascular Screening of High School Athletes: A Prospective Study, J Am Heart Assoc. 2019; 8:e012235. DOI: 10.1161/JAHA.119.012235.
- Ghani S, Et al., Cardiovascular Medicine 2012; 15(1):7-13
- Harmon KG, Zigman M, Drezner JA. The effectiveness of screening history, physical exam, and ECG to detect potentially lethal cardiac disorders in athletes: a systematic review/meta-analysis. J Electrocardiol. 2015;48:329–338.
- Bronzetti G et al., Chronicle of a death foretold. It is time for echocardiographic screening in young athletes, American Heart Journal Plus: Cardiology Research and Practice, Volume 8, 2021, 100038, ISSN 2666-6022, Whttps://doi.org/10.1016/j.ahjo.2021.100038.
- Mont L et al., Pre-participation cardiovascular evaluation for athletic participants to prevent sudden death: Position paper from the EHRA and the EACPR, branches of the ESC. Endorsed by APHRS, HRS, and SOLAECE, EP Europace, Volume 19, Issue 1, January 2017, Pages 139–163, https://doi.org/10.1093/europace/euw243
One thought on “Preventing Sudden Cardiac Death in Athletes: The Role of ECG and Echocardiogram in Sports Screenings”